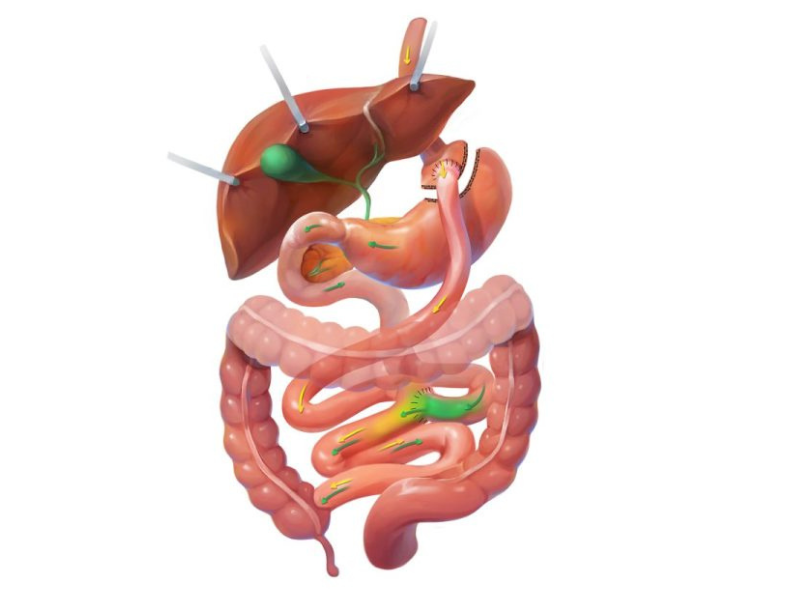
The gastric bypass combines restriction and malabsorption. The amount of food a patient consumes is restricted by the reduced size of the stomach, and calorie absorption is reduced by bypassing part of the intestinal tract. The first phase of surgery involves cutting away approximately 85% of the existing stomach. The remaining usable stomach pouch is about the size of a golf ball. The larger part of the stomach remains in the abdomen, receiving no food, but contributing digestive juices further down the digestive tract.
The second part of the procedure bypasses a portion of the small intestine, reducing the surface area of the intestine exposed to food and limiting caloric absorption.
As with most bariatric surgery procedures today, including the gastric sleeve (sleeve gastrectomy), the gastric bypass is performed in a minimally invasive manner using four or five small incisions in the abdomen, rather than the traditional open surgery that employs a large single incision. The procedure can also be performed with our surgical robot’s assistance. Procedures are typically performed in a hospital setting and require an overnight stay.